Surgical procedures
- Лапароскопия аппендицита
- Геморрой
- Грыжи
- Доброкачественные образования кожи и ПЖК
- Желчнокаменная болезнь
- Эпителиальный копчиковый ход
- Парапроктит

Laparoscopy appendicitis
Laparoscopy appendicitis is a surgical operation that is performed through a relatively small hole. In modern medicine, laparoscopic appendectomy is popular, because this method has some advantages compared to open surgery for appendicitis. The advantages of laparoscopic appendectomy compared to open surgery, laparoscopic appendectomy has several advantages: postoperative pain is significantly reduced intensity; the motility of the intestines is restored at an early date; the cosmetic effect after the operation is obvious: remains of the scar from appendicitis; the length of stay in hospital is significantly reduced; the ability to work patient recovers in a short time.
General contraindications for surgery of this type: before undergoing surgery, obesity, and increased bleeding; severe hemorrhagic diathesis, hemophilia, intolerance to anesthesia, the later stages of pregnancy. Local contraindications are: generalized peritonitis and intestinal adhesions; retroperitoneal abscess, revealing a dense appendicular infiltrate, in the absence of the Appendix signs of inflammation.
Preparing for surgery for appendicitis. Since laparoscopy appendicitis is a planned operation, then it is preceded by a thorough examination of the patient, number of laboratory tests, ultrasound diagnostics of abdominal cavity and small pelvis.
Possible complications of laparoscopy appendicitis. Laparoscopic appendectomy can cause some complications of acute appendicitis, which is divided as follows: intraoperative complications: the intersection process of the ligature, damage to the bowel, bleeding from the appendicular artery, damage to a trocar intestine; postoperative complications: education in the field of introduction of trocar hernia, hematoma of the anterior abdominal wall, festering wounds on the skin, common postoperative peritonitis, abdominal abscesses, dehiscence and necrosis of the stump of the Appendix, intra-abdominal bleeding.
The post-operative period. One of the main advantages of laparoscopic appendectomy is a very short postoperative period. Patient compliance with prescribed bed rest from 4 to 24 hours, careful implementation of special gymnastics, antibiotic therapy, diet food.
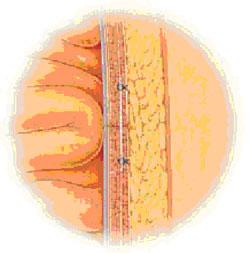
Hemorrhoids
Hemorrhoids are associated with pain, hemorrhoids bleeding, prolapsed hemorrhoid. In typical cases a small bleeding occurs during or immediately after defecation (bowel movement). The color of the blood usually scarlet, but perhaps the release of dark blood, sometimes with clots. Regular discharge of blood pretty quickly leads to anemia (anemia). Prolapsed internal hemorrhoids often evolves gradually. Initially appears during defecation, after some time, straining, lifting, coughing, sneezing. In the early stages the nodes are easy to reduce in the future reside outside the anal canal (outside). At any stage of possible thrombosis and necrosis of the haemorrhoid with the development of severe clinical picture.
Complication is bleeding, acute suppurative abscess, and necrosis.
Early stages of the disease enough are treatment, but the 3-4 stage of hemorrhoids without surgery to cure it completely is very difficult. At this stage the most effective way of treatment is surgery Milligan-Morgan. With this method you can get rid of annoying and dangerous diseases forever.Hernia
Symptoms of a hernia can be:
- A feeling of weakness, pressure, burning or pain in the abdomen, groin or scrotum.
-
The presence of bulges or bumps on the belly, in the groin or the scrotum that protrude when you cough and disappears in the supine position.
-
Pain when straining, lifting or coughing.
Upon confirmation of the diagnosis of a hernia are often recommended the surgery.
Accompanied by a short recovery period with minimal discomfort in the postoperative period.
Without treatment hernias can cause emergency conditions.
When compression of tissues outside of the abdominal wall hernia becomes irreducible. Upon termination of the blood supply of the compressed bodies, the hernia becomes strangulated. In strangulated hernia, the tissues swell, become infected and die quickly. This requires immediate medical attention.
-
If You have a hernia and nausea, vomiting; the appearance of blood in the stool, and in the absence of bowel movements and flatus.
-
If You have a rapidly increasing pain in the groin or the scrotum.
- If the hernia does not reduce easily in the supine position.
What really is the cause of the formation of hernia?
You may have increased risk of hernia if You:
-
suffer from a chronic cough, such as smoker's cough;
- overweight;
- often make an effort at defecation or urination;
- suffered pregnancy;
- often tense lifting weights;
- often sneeze, such as allergies.
Different types of hernias and where they occur

If You suffer from inguinal hernia, You are not alone. Inguinal hernias are the most common type of hernia. This type of hernia is more common in men than in women.
This is due to the fact that this type of hernia occurs in the natural weak spot of the abdominal wall, the so-called inguinal canal. If You are a man, Your testicles must descend through the inguinal canal before birth. Due to the omission of the eggs is formed by a natural defect called the internal inguinal ring, in the area which can form a hernia, if the ring will not be compressed sufficiently. Hernia, formed in this region are called inguinal, there are two types of inguinal hernias: direct and oblique.
Oblique inguinal hernia passes through the internal inguinal ring, are the most common and is found in 2/3 of all cases. Direct inguinal hernias are formed when the weakness of the lower wall of the inguinal canal and are more likely to develop in men over the age of 40 years. The bottom wall of the inguinal canal is located directly below the internal inguinal ring.
Epigastric hernia is another type of hernia that is more common in men than in women. Hernias of this type are located above the navel in the upper abdomen in the midline.
There is one type of hernia that is more common in women than in men - a femoral hernia. Hernias of this type are placed immediately under the groin crease and are usually formed as a result of pregnancy and childbirth. Weakness in the lower groin area causes an exit of the loops of intestine through the femoral canal, the space around the femoral vein, which collects blood from the lower limbs
If You have had surgical operations on the abdominal organs, You may have increased risk of incisional or ventral hernias. Hernias of this type can be formed in the operating region of the scar after weeks, months and even years. If You think You have an incisional hernia, You should consult your doctor. Without treatment hernias can increase in size, and their treatment can be extremely difficult.
We all have a natural weak spot in the abdominal wall. Is the area around the navel, where the umbilical cord joined before you were born. Umbilical hernias are located around the navel and meet the men, women and children. Sometimes they can form due to increased pressure in the abdominal cavity due to excess weight, a strong cough or pregnancy.
The treatment of hernias
Currently, surgeons use several types of surgical operations for hernias. Your doctor may offer one or several types of surgery to choose from. Understanding all the capabilities will help You to choose the most suitable type of surgery.
Hernia repair with tissue tension
For a long time, the hernia repair with tissue tension was the only treatment for hernias. During surgical intervention of this type, the surgeon cut through the abdominal wall over the hernia, moved out-of abdominal tissue back and then sutured the abdominal wall. Currently hernia repair with tissue tension is applied only in children and hernia of very small size. The main disadvantages of hernioplasty with tension fabrics are:
-
Discomfort.
-
The recovery period is 4-6 weeks.
-
There is a 10-15% chance that a hernia will appear again.
Hernia repair without tension of the tissues
Currently, the hernia repair without tension of the tissues is more common treatment. Likely Your physician will recommend one of the following methods of treatment. We describe the most common 5 methods of hernia repair without tension of the tissues
Hernia repair using mesh flat
After the skin incision over the hernia, the surgeon sews a patch made of flat plastic (polypropylene) mesh to the tissues surrounding the place of hernia.
Advantages:
Recurrence of hernia was noted only in 3% of patients undergoing hernia repair using a plastic mesh.
• A rapid recovery.
• Low degree of discomfort after surgery.
• The operation can be performed under local anesthesia.
Disadvantages:- Hernia of large size is necessary to impose a greater number of seams, which increases the risk of nerve damage.
- The operation can last from 40 to 60 minutes.
Operations with the use of occlusive and flat implants
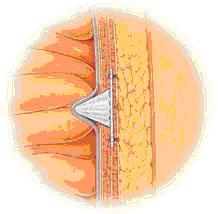
Commonly used in the treatment of inguinal hernias, this technique is similar to a hernia repair with the use of the flat mesh.
Advantages:
The same as when using a flat mesh.
Disadvantages:
Well enough protects against the formation of new hernias.
Occlusive implant may decrease in size, which increases the risk of:
- development of recurrence;
- shift occlusive implant.
Some patients have marked discomfort due to the fact that they feel occlusive implant through the skin.
Laparoscopic surgery
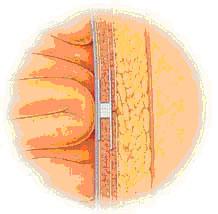
In laparoscopic surgery the surgeon through a small incision introduces into the abdominal cavity a laparoscope (a thin instrument with a light source and magnifying lenses). The laparoscope allows the surgeon to examine the place of hernia and mesh enter the abdominal wall.
This type of operation is called hernioplasty back. It differs from traditional methods of hernioplasty using meshes (described above), in which the mesh is attached from the external side of the abdominal wall.
Advantages:
The pressure inside the abdominal cavity holds the mesh in place.
Disadvantages:
Intervention should be performed under General anesthesia, which is the most risky stage of any surgical operation.
You may need a one-day hospitalization in a medical facility.
The duration of the operation can be 60 minutes.
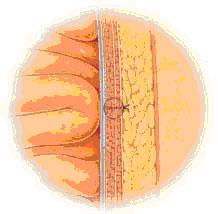
Hernia repair using mesh having a three-dimensional configuration
The latest technology of surgical treatment of hernias combining the advantages of the previously developed methods of treatment of hernias tension-free tissues. A new device (PROLENETM Hernia System, manufactured by Ethicon Inc., Johnson & Johnson company). The system consists of three components:
internal flap which provides a secure fit with the inner side of the abdominal wall;
fittings, having the form of a tube;
"lining" (outer flap) that covers the abdominal wall.
Advantages:- High degree of comfort.
- The almost complete absence of the possibility of offset and the development of recurrences. To date, no information on the development of recurrence in more than 50,000 patients undergoing surgery with the use of a grid having a three-dimensional configuration.
- A small number of overlay sutures reduces the risk of nerve damage.
- The operation can be performed under local or regional anaesthesia.
- The operation lasts about 20 minutes.
- Short recovery period.
- Your surgeon may not have the skills to use the grid having a three-dimensional configuration.
The recovery period after surgery for hernia
After surgery, You can be assigned to anesthetic, if You have discomfort in the area of operating wound. The incision will be closed with a bandage. Ask your doctor or nurse when You should take off the blindfold. In most cases, You will be able to leave a medical facility soon after surgery. Perhaps the staff of the medical institution will want to ensure that You feel well enough to go home, and if You can eat, drink, move around and not broken if You have urination. Driving a car may be associated with the load operation zone, so Your doctor may ask You to withdraw for a while from driving. This is another reason why You need someone's help, at least in the first days after surgery. Perhaps during the first days after surgery, You will notice the presence of swelling or discoloration of the skin in the area of operations. Also not a deviation from the norm, the presence in the area of operation of the bruises, sensitivity or, conversely, reducing or numbness.
During the recovery period after surgery will depend on Your health condition and the type of surgery performed Your doctor. After discharge from the hospital back to their regular activities gradually. Time to go back to work depends on the nature of Your work. If Your work involves physical effort e.g., lifting, for full recovery may require several weeks. To work associated with physical labor You will be able to return after three days. Be sure to consult with your doctor on the timing of the return to work.
Moderate exercise, such as walking, helps to normalize circulation and increase the rate of wound healing. It is important to prevent the development of constipation, which increases the load on the area of the wound. Follow a diet rich in dietary fiber, drink plenty of fluids - water and fruit juices.
When to call your doctor
If You have to return home have any of the following re-numerical problems, contact your doctor
-
Fever.
-
Severe swelling (swollen small size is the norm).
-
Redness.
-
Bleeding.
-
The increasing pain.
Before surgery You may be asked to:
Stop taking all drugs, including over-the-counter, such as aspirin and tylenol.
To quit Smoking, to avoid strain on the area of the hernia caused by cough, and to normalize blood circulation to accelerate healing of surgical wounds.
To avoid heavy lifting that can affect a hernia
Do not eat or drink for several hours before surgery to prevent vomiting during the operation.
Upon admission to the hospital the day of surgery will be carried out the following activities
You sign the informed consent form, if You haven't done this before.
You will be measured blood pressure, pulse and temperature.
Your doctor or anesthesiologist will explain to You what type of anesthesia will be used during the operation. Agree with someone who could get You home from the hospital and would provide You assistance in the home immediately after the operation.
Possible complications in operations for hernias of are:
-
Bleeding.
-
Infection.
-
Pain or loss of sensation.
-
Difficulties when urinating.
-
Pronounced bruising.
-
Swelling in the groin or swelling of the testicles.
-
Recurrence of the hernia.
- Complications due to anesthesia.
Make sure that You sign the informed consent, only those interventions that you have discussed with your doctor.
Prevention of hernias
There is no method of prevention of hernias. A hernia can develop in any person. The best thing You can do to prevent the development of hernia is to lead a healthy lifestyle:
Eat right. This will prevent the development of constipation, which cause a stretching of the intestine. In addition, nutrition supports the muscles in a healthy condition.
Do not smoke. If You smoke, quit. Chronic cough due to irritation of the lungs increases the risk of hernia. Chronic cough increases the risk of recurrent hernia. Get regular moderate exercise to maintain the abdominal muscles in shape. Maintain a healthy weight. If You are overweight, try to lose weight to reduce the load on the muscles of the abdominal wall. Use proper lifting techniques, do not lift too heavy objects.
Exercise for the Prevention of Abdominal Hernia
What can You do to prevent the development of hernia? Try to strengthen abdominal muscles: lie on your back, bend your knees and place your feet on the floor. Without lifting your shoulders off the floor, raise your buttocks and back. Repeat ten times.
Benign skin and subcutaneous fat
Our clinic provides services of removal:
- Lipomas (fatty tumor, fatty lipoma — a benign connective tissue tumor, developed in the loose layer of subcutaneous connective tissue and can infiltrate between the muscle and vascular bundles to the periosteum. Is characterized by a Tumor of soft consistency, painless and easily movable. Grows slowly. Lipoma is more common in places with poor adipose tissue: upper back, shoulder girdle, the outer surface of the shoulder and hip. Lipoma is not dangerous. Lipomas in the subcutaneous adipose tissue regenerated infrequently (liposarcoma).
- Atheroma (tumor formation arising from blockage of sebaceous gland duct). Is characterized by: defined superficial dense-elastic formation with clear contours, mobile. The skin over the formation of the fold is not going to. When suppuration of sebaceous cysts be pain, redness, swelling, tenderness, fever, fluctuation; the atheroma can break out pus with a similar fat content.
- Genital warts. Is characterized by: are small flesh-colored growths that can appear on the genitals, around the anus, sometimes in the mouth.
- Gigram (accumulation of serous-mucous or sero-fibrinous fluid in the cavity or the newly formed periarticular synovial bags, having the appearance of tumor formations). Is characterized by: clinically, this tumor is a rounded shape, good thickness, covered with normal skin, with a diameter of from 0.5 to 3 cm, movable, though fixed at the base.
- Hemangiomas (common benign vascular education). Is characterized by: Simple hemangioma are red or blue-purple color, is disposed on the surface, clearly delimited, affects the skin and a few millimeters of subcutaneous fat layer grows mainly in side. Surface hemangiomas are smooth, less rough, sometimes slightly protruding above the skin. When pressing the hemangioma fades, but then again restore its color. Cavernous hemangioma is beneath the skin in the form of a restricted site. Looks like tumor formation, covered with unaltered or bluish on top of the skin. When pressed hemangioma collapses and fades (due to the outflow of blood). Combined hemangioma are a combination of superficial and subcutaneous hemangiomas (simple and cavernous). Combined hemangioma is composed of tumor cells emanating from blood vessels and other tissues. Appearance, color and texture are determined by members of the vascular tumor tissue.
Cholelithiasis
This disease is justly considered a "disease of the century" and a "disease of prosperity," referring to a direct connection of its development with the nature of power. Over the last decade has dramatically increased the incidence of cholelithiasis. More common in people whose work is associated with psychological and emotional stress and sedentary lifestyle.
In a well-functioning supply system of the bile the body has one weak spot: when there is a concentration of bile in the bladder, there is a risk of stagnation with the formation of clots, and then stones. Gallstones are crystalline structures that occur in abnormal bile. The stones are different depending on the preponderance of components of bile: cholesterol (occur in 80-85% of patients), pigmented and mixed.
The high content of cholesterol in bile and promotes the growth of stones. This process is lengthy: it may take several years of Cholesterol stones is the acquisition of the population of developed countries, especially those with overeating. With a vegetarian diet cholelithiasis is rare.
The reason for the development of Gallstones is not a mechanical disturbance of outflow of bile in the bile ways - dyskinesia.
Dyskinesia can manifest in the form of spastic contractions of the gallbladder and in the form of its atony with the stagnation of bile. Initially, changes may be purely functional in nature. Then there is the inconsistency of the action of the bladder and of the sphincter that is connected with the violation of innervation and humoral regulation of motor function of the gallbladder and biliary tract. The disturbance of this mechanism is when vegetariana, inflammatory diseases of the gastrointestinal tract, violation of rhythm and power.
Distinguish GSD:
uncomplicated, or kunenalatest, when with the exception of stones other symptoms of the disease not;
complicated when there is at least one complication( inflammation of the gallbladder, bile duct stones, inflammation of the pancreas).
Due to a common blood supply, innervation, topographical proximity in the pathological process involved in GSD hepatobiliary, gastroduodenal system, pancreas, intestines.
Clinic gallstone disease is extremely diverse. It largely depends on the number of stones, their location and magnitude, and also from the Department of the biliary system, where the calculus gets "stuck". In a sufficiently large number of patients with the presence of stones in the gallbladder no symptoms of the disease there usually is a single, large stones. This latent form of the disease.
A typical manifestation of gallstone disease are biliary colics, due to the release of stones from the bladder and the promotion of their ducts. Themselves pain due to spastic contractions of the bladder, increasing pressure in it. The pain occur suddenly, are localized in the right upper quadrant and very often in the epigastrium, radiating to right arm, right shoulder, accompanied by nausea, repeated vomiting, which does not bring relief. Characterized by localized pain - at the point of the gallbladder and in the right hypochondrium. Often seen after intake of fatty, fried, spicy food, cold soda water, beer. The pain can be different: pain, stupid, tolerant (in remission); sharp, unbearable pain (in the acute stage), which can be triggered by jolting, riding, wearing of severity, sometimes associated with emotional tension.
- The syndrome of dyspepsia. Occurs as a result of throwing the bile into the stomach. There is a feeling of bitterness in the mouth, sometimes heaviness in the epigastrium. Rarely joins nausea, vomiting.
- Intestinal dyspepsia: the tendency to flatulence, sometimes intolerance to dairy diet, frequent diarrhea, less constipation. When holetsistopankreatit typical liquid foul-smelling stools. Often reflux from the duodenum into the stomach, accompanied by a subjective feeling of bitterness in the mouth. As a result of bile reflux, there is a gradual atrophy of the gastric mucosa.
- The diagnosis of cholelithiasis is established on the basis of anamnesis, data of objective inspection of the patient, data of laboratory parameters, ultrasound examination of abdominal cavity.
In many modern manuals of ultrasound diagnosis is the gold standard technique in the setting of cholelithiasis.
Pain in gallstones quite well docked when using antispasmodics, antifermental, antisecretory drugs. The presence of stones in the gallbladder and at least 2 attack of biliary colic per year are an indication for surgical treatment. It should be noted that elective surgery should preferably be done in the cold period ie during remitting pain. The gold standard in the surgical treatment of cholelithiasis is laparoscopic cholecystectomy. Method to delete a bubble using 4 small puncture in the abdominal wall bypassing the classic large incisions.
Pilonidal sinus disease
Pilonidal sinus disease is a congenital defect (a narrow tubular cavity) in the tissues of the sacrococcygeal region. Sometimes pilonidal sinus disease called dermoid cyst of the coccyx, pilonidal sinus, they hiss coccyx.
Primary epithelial coccygeal passage opens to the skin of the buttocks (in mezhyagodichnoy fold) one or more small holes, the other end terminates in the subcutaneous tissue and has no communication with the sacrum or tailbone.
Periodically through point outputs coccygeal fistula allocated to the waste products of its lining epithelium. In addition, through these holes in the fabric can penetrate the infection.
Pilonidal sinus disease is a long time not seen clinically. Patients are turning to the surgeon, usually when inflammation of the Epithelial pilonidal sinus.
The symptoms of pilonidal sinus disease
In the first years of life pilonidal sinus disease does not manifest itself. During pubertal period starts during hair growth, the allocation of metabolic products of the epithelial lining (sebaceous, sweat glands). This can result in itching, oozing due to discharge from pilonidal sinus disease. The location of the exit of the epithelial pilonidal sinus near the area of the anus, the increased moisture in mezhyagodichnoy the crease, active skin glands contribute to the blockage move, and stagnation of the content contributes to the development of infection. Factors contributing to the inflammatory process in the coccygeal the course are: increased body hair area of primary holes, the violation of hygienic rules, injury, scratching.
Inflammation of the epithelial pilonidal sinus is characterized by pain in the sacrum, sometimes sukrovichnye or purulent discharge. Often patients assume that the symptoms a consequence of injury. Originally developing an acute inflammation, the infiltrate is formed, and then purulent abscesses. At this time, if a patient goes to the doctor, made the necessary remedial measures to remove the pilonidal sinus disease, then recovery occurs. If access to a doctor was not followed in time, often there is a spontaneous opening of the abscess on the skin. This usually occurs after pain relief, however, most often an infectious lesion persists, leading to chronic inflammation. Formed purulent fistula connecting the cavity of the abscess with the skin, the disease runs in waves, relapse of suppuration. The existing chronic inflammation gradually encompasses more and more area, increases toxicity in the body.
Diagnosis of pilonidal sinus disease
Pilonidal sinus disease is not difficult to diagnose, its identification is usually sufficient for the detection of primary holes in between the gluteal fold.
In rare cases, the need of differentiation of the pilonidal sinus disease from another disease, produce fistulography.
Treatment of pilonidal sinus disease
Pilonidal sinus disease treated only by surgery. Surgery involves a radical removal of the pathological channel with the primary holes. In the case of complicated epithelial stroke excised and pathologically altered surrounding tissue, purulent fistula.
As prevention measures of postoperative recurrence make removal of the hair around the wound and then around the scar.
Paraproctitis.
According to statistics, the abscess occupies the fourth place in the overall structure of a variety of kidney diseases. More common than acute and chronic paraproctitis meet only such diseases as colitis, anal fissures and hemorrhoids. Scientists estimate that out of a hundred patients who have come on reception to the proctologist, from 20 to 40 people suffer from such problems as the abscess, and most of them were men.
What is Paraproctitis?
Occurs abscess due to bacteria, such as enterococci, staphylococci, E. coli and anaerobic bacteria. In adipose tissue the infection enters from the lumen of the rectum due to cracks in the anus or due to damage to the mucosa. The gateway for this infection are most often morganeve crypts. Somewhat less often, the bacteria penetrate the boils, wounds, and also from the prostate gland (when it is inflamed). Sometimes the infection is hematogenous through the bloodstream from another source of inflammation.
For this pathology as an acute abscess is characterized by the sudden beginning and strongly expressed clinical manifestations. The signs in this case will depend on exactly where localized inflammation, what are its dimensions and what is the state of immunity. Despite the fact that there is a classification of forms of this disease, there are symptoms that are common to all its species:
-
pain of varying intensity in the pelvic area, lower abdomen, in the rectum, which worsens during defecation;
-
-
disorder urine and stools, which is manifested as painful urination, painful urination, constipation;
-
the rise in temperature to 38-39 degrees, which is often accompanied by chills;
-
General intoxication: malaise, weakness, aching joints and muscles, loss of appetite and headaches.
The main purpose of surgical operations for the treatment of acute paraproctitis is a purulent destruction of the masses, as well as the establishment and full removal of anal crypts and glands, with which the inflammatory process has begun. However, diagnostic situations can be different.
After the operation for chronic or acute abscess requires power adjustment. Usually no special diet is required: to eat gentle food is mostly boiled or steamed. Spicy, fatty, spicy foods should be abandoned. After plastic surgery for paraproctitis is assigned to the food to soften the stool. Need to consume dairy products, dried fruits, and limit fresh fruits and vegetables, carbonated drinks, strong coffee, tea, chocolate.